Joint Care: Knee and Hip Replacement Surgery | Sports Medicine | Spine and Back Pain
A commitment to excellence in orthopaedic patient care is backed by a growing emphasis on clinical research. Our dedicated orthopaedic research investigators, with the support of the NorthShore Research Institute, work on a growing portfolio of collaborative research projects across disciplines, creating a ‘bench to bedside’ atmosphere that offers the latest technology and care, ensuring that our patients have access to the most advanced treatment options.
Joint Care: Knee and Hip Replacement Surgery
Our Joint Care: Knee and Hip Replacement Surgery program routinely collect information from patients on the outcomes of their joint replacements. Additionally, working closely with Health Information Technology, the group integrates the collection of important clinical data with the use of our Electronic Health Record, Epic. This allows us to track patients and their outcomes and leverage this data for a variety of studies aimed at improving care. NorthShore is participating in the American Joint Replacement Registry which allows our physicians to track data on a complete range of devices and techniques and monitor performance and trends locally and nationally. Outcomes data will be studied and applied to best practices going forward for device design and surgical methods.
Researchers in Pharmacogenomics, Anesthesia and Adult Reconstruction are partnering to look at how an individual’s genetic profile may affect their pain control following total knee replacement surgery. The ability to control a patient’s post-operative pain, using a personalized approach, would minimize opioid use and have a positive effect on patient outcomes.
Sports Medicine
Our Sports Medicine team is leading the way in safety and quality improvements for shoulder surgery and other orthopaedic procedures by collecting patient reported outcomes on our shoulder and sport’s knee patients. This data collection, along with the use of the electronic medical record, improves our ability to monitor patient outcomes, engage in research studies and improve care.
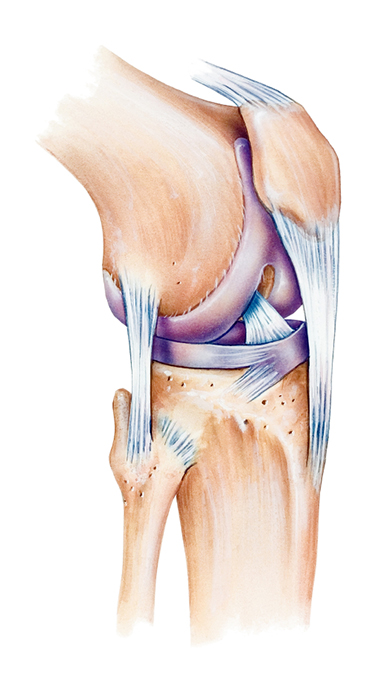
Advances in knee surgery are proving fruitful as well. Our surgeons are using regenerative medicine as a technique to regrow cartilage to heal knee injuries. The process involves taking healthy cartilage from a patient, growing the cells in the lab and then transplanting the cartilage cells back into the patient’s knee. Cartilage has no ability to heal, but regenerative medicine enables cartilage to regrow in patients, and in many cases improves patients’ outcomes. Patients typically return to an active life within months of the procedure.
The Department of Orthopaedic Surgery received an award in 2018 from the Women’s Auxiliary Fund to pursue regenerative research. The knee osteoarthritis study compares the use of two types of treatments; use of a patient’s platelet rich plasma versus the standard of care treatment to stimulate a patient’s cartilage growth.
NorthShore and researchers from the Hospital for Special Surgery and Cincinnati Children’s Hospital are working together to study patella instability and dislocation in patients less than 30 years of age. This condition can be devastating to young patients, causing pain, loss of function and potential arthritis. Results of nonoperative and various surgical treatment outcomes will be compared, including assessment of function, activity and quality of life.
Spine and Back Pain
Our Spine and Back Pain team is pursuing research related to spinal instability. Dr. Mark Mikhael is researching the use of donor stem cells to help facilitate fusion during spinal surgery. Known as spondylodesis, spinal fusion is a surgical technique used to join two or more unstable vertebrae. In adults, supplementary bone tissue cells are used to help the body’s natural bone growth fuse the vertebrae together. Instead of retrieving the patient’s own stem cells, traditionally obtained by taking a portion of bone from the patient’s hip though a separate incision, surgeons are testing the use of donor stem cells to stimulate bone fusion. For the patient, this prevents additional pain, blood loss, surgical time, risk of infection and delayed recovery associated with surgery.