Below are frequently asked questions about all facets of diabetes. Use the links below to jump to the section that interests you.
Diabetes Testing | AC1 | Glucometer | Blood Sugar Levels | Insulin | Diet | Exercise | Sick Days | Family Planning | Sharps | Medical Alert Identification | Continuous Glucose Monitoring | Resources
Diabetes Testing
How does a physician diagnose diabetes?
- There are three types of blood tests doctors can use to determine if a patient has diabetes:
- A1C test, which measures average blood sugar over the last 3 months
- Fasting plasma glucose test measures blood sugar levels after fasting for at least 8 hours
- Oral glucose tolerance test, measures blood sugar 2 or 3 hours after eating—often used to diagnose gestational diabetes (3 hours), and is one of the ways to diagnose type 2 diabetes (2 hours)
| Blood Test |
What It Measures |
Without Diabetes |
With Pre-Diabetes |
With Diabetes (Type 1 or 2) |
| Fasting plasma glucose |
Blood sugar levels fasting > 8 hours |
< 100 mg/dL |
100-125 mg/dL |
> 126 mg/dL |
| Oral glucose tolerance test |
Blood sugar levels 2 hours after eating (often used to diagnose gestational diabetes) |
< 140 mg/dL |
140 - 199 mg/dL |
> 200 mg/dL |
| AC1 |
Average blood glucose over 2-3 months |
< 5.7 (average blood glucose range < 100 mg/dL) |
5.7-6.4 (average blood glucose range = 117-137 mg/dL) |
> 6.5 (estimated glucose number = 140 mg/dL) |
AC1
What is the A1C test?
- The A1C test (glycated hemoglobin) measures a person’s average blood glucose level over the last two months in pregnant patients and three months for non-pregnant patients. The A1C also can be reported as an estimated average glucose value. People with diabetes should get their A1C tested every 3-6 months.
| AC1 % |
eAG mg/dL |
| 5 |
97 |
| 5.5 |
111 |
| 6 |
126 |
| 6.5 |
140 |
| 7 |
154 |
| 7.5 |
169 |
| 8 |
183 |
| 8.5 |
197 |
| 9 |
212 |
| 9.5 |
226 |
| 10 |
240 |
| 10.5 |
255 |
| 11 |
269 |
Why is having a well controlled A1C important?
- Higher A1Cs are correlated with many diabetic complications such as heart disease, kidney failure, neuropathy (nerve damage), erectile dysfunction and retinopathy (eye damage). This means that patients with uncontrolled diabetes are at higher risks for heart attacks, dialysis, blindness and amputations. Working with your healthcare provider can help prevent these outcomes.
Glucometer
What is a glucometer?
- A glucometer (or “glucose meter”) is a device used to monitor a person’s blood sugar at a particular moment in time. It is important to use a glucometer throughout each day to keep track of blood sugar.
Why keep a blood sugar logbook?
- It is also important to keep a detailed blood sugar logbook to see “trends” in blood sugar.
Blood Sugar Level
What is hyperglycemia and hypoglycemia?
- High blood sugar is called hyperglycemia, whereas low blood sugar is called hypoglycemia.
What are the consequences of hyperglycemia/hypoglycemia?
- Prolonged hyperglycemia can lead to vomiting, excessive hunger and thirst, vision problems and rapid heartbeats, as well as even more serious complications like diabetic ketoacidosis (also known as DKA). DKA is a serious and life-threatening complication if left untreated. Hyperglycemia can be managed by improving one’s behaviors through being physically active, managing one’s eating habits, staying hydrated and medication as needed.
- Prolonged hypoglycemia can lead to premature death of brain cells, causing damage to memory, learning and other brain impairments. Hypoglycemia is also a cause for falls, fractures, dementia and heart attacks. To treat hypoglycemia, one should follow the rule of 15. If blood sugar is below 70, treat it with 15 grams of fast-acting glucose.
Insulin
What is insulin?
- Food is broken down into a variety of nutrients, including carbohydrates (sugar), which is used as fuel in cells. Insulin is a hormone that is created in the pancreas that glucose needs in order to move from the bloodstream into cells. Insulin is important because it lowers blood sugar and helps keep it within normal levels. Without insulin, glucose stays in the bloodstream, which leads to high blood sugar readings.
- When a person has diabetes, the pancreas cannot properly create insulin or process sugar, leading to erratic and uncontrolled blood sugar levels if no intervention is taken.
How to take insulin
- Insulin is an available option as an injectable medicine, and is a lifesaving tool for people with diabetes. There are two main ways of delivering insulin to your body: through a pen and through a syringe.
Diet
How do diabetes patients adjust eating habits?
- There is no one-size-fits-all approach to meal planning for patients with diabetes, and as a result patients diagnosed with diabetes should meet with a certified diabetes care and education specialist to help craft an individualized meal plan to meet their specific needs.
What is nutritional therapy?
- The goals of medical nutritional therapy are to support healthy eating patterns and improve overall health by:
- Attaining personal weight goals
- Attaining personal blood sugar and cholesterol goals
- Delaying or preventing complications of uncontrolled diabetes
Can diabetes patients drink alcohol?
- No more than one an hour (2 to 3 drinks a night) and always with food. Otherwise it will cause low sugars.
Exercise
How often should diabetes patients be exercising?
- The American Diabetes Association (ADA) recommends at least 150 minutes of exercise each week, which is about 20 to 30 minutes of physical activity most days of the week. Recent evidence supports that all individuals, including those with diabetes, should be encouraged to reduce the amount of time sedentary by breaking up activates that may require lengthy sitting times.
- The ADA also recommends at least 2 weekly sessions of resistance (using resistance bands or free-weights), 2-3 times a week spent on flexibility and balance training, and stretching daily.
When should a diabetes patient begin an exercise routine?
- Check with your doctor before beginning an exercise routine. Once cleared, it is healthiest to start small and build up from there. Start with 3 days of 15 minutes of exercise, and each week add an additional day or an additional 5 minutes to the daily amount of exercise.
- For blood sugar guidelines before exercising, please refer to the Diabetes Owner’s Manual.
Sick Days
How do sick days affect diabetes patients?
- When sick, injured or have an infection, the body is under stress. It responds by releasing hormones. These hormones can cause high blood sugar levels and make it harder to get well.
How should a diabetes patient handle a sick day?
- Be prepared before getting sick.
- Talk with your diabetes care team about the following:
- getting a flu shot every year
- a sick-day menu
- liquid carbohydrates to have on-hand in the event of nausea or vomiting
- extra diabetes supplies
- Find out how frequently you should check your blood sugar levels during a sick day. Keep a list of telephone numbers that include your doctor, your certified diabetes educator and your pharmacy. Always have a list of your current medications available.
- Drink plenty of liquids.
- Drink 8 ounces of water or other calorie-free beverages every hour. You also can have ice chips, sugar-free popsicles, sugar-free soda, sugar-free Jell-o and clear broth.
- If unable to eat, drink liquids that contain sugar.
- Choices include fruit juice, regular soda and sports drinks.
- Check blood sugar frequently—on average at least every 4 hours.
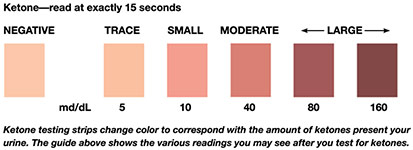
- Check your urine for ketones if blood glucose is greater than 240 mg/dL.
- Continue to take medication and insulin.
- If you have nausea or diarrhea, check with your doctor or certified diabetes educator to find out how to adjust your medication doses.
- If taking meal time insulin and unable to eat, do not take that insulin.
- If on an SGLT2 test your ketones and call your doctor.
When should a diabetes patient call the office during a sick day?
- Here are symptoms to watch for when you are sick. If you experience any of them, you need to call your doctor for immediate medical attention.
- Inability to keep liquids down for more than four hours
- Vomiting or dehydrated
- Diarrhea or abdominal pain
- Difficulty breathing or have fast breathing.
- Blood glucose is over 300 mg/dL on 2 consecutive measurements that do not respond to increased fluids or food, or is over 350 mg/dL once
- Blood sugar levels are too low
- Ketones in urine
- Temperature of 100.4 F (38C) or above
- Confusion or unable to stay awake or think clearly
- Breath smells fruity or like fingernail polish remover
Family Planning
How should a diabetes patient plan for a family?
- It is important to plan pregnancies ahead of time, when possible. Work with your doctor to ensure you are being safe while trying to become pregnant, and to discuss making any necessary changes to medicines to help achieve pregnancy. Your doctor also will instruct you on how to monitor kidney and eye health.
- As a general rule, when trying to become pregnant, A1C should be less than 6.
Sharps
How should one properly dispose of sharps?
- Sharps from needles can cause injury if not properly disposed of. Here are organizations that provide education and manage disposal of sharps:
Medical Alert Identification
- It is advised for individuals with chronic illness such as diabetes to have a medical alert identification to help facilitate care in case of emergency.
- They are available from pharmacies or the internet, and it is recommended to note that you are a diabetic, what type, if you’re on insulin and other medical issues.
Continuous Glucose Monitoring
What is a CGM and why does it make my life easier?
- Continuous glucose monitors (CGMs) are devices that provide real-time glucose readings, throughout the day and night, enabling people with diabetes to see their blood sugar levels and track how quickly they are increasing or decreasing. Some new CGMs (such as the Dexcom G6 and Freestyle Libre) don’t require calibration with fingerstick and may minimize the need for monitoring with your glucometer.
Cost and coverage for CGMs
- For costs of individual CGM systems, as well as coverage for these systems, check with the manufacturer on their website for more information. Medicare will cover patients with diabetes on multi-dose insulin.
Resources
Manuals & Programs
Apps and Online Resources